-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Christopher Emmanuel Makam, Awolu Adam* and Adam Fusheini
Corresponding Author: Awolu Adam, Department of Family and Community Health, School of Public Health, University of Health and Allied Sciences, Ho, Ghana.
Received: April 01, 2022 ; Revised: April 21, 2022 ; Accepted: May 14, 2022 ; Available Online: May 20, 2022
Citation: Makam CE, Adam A & Fusheini A. (2022) Self-Medication and Pregnancy Care: The Use of Herbal Products and Prescription Drugs Among Pregnant Women Attending Antenatal Clinics in Hohoe Municipality of Volta Region, Ghana. J Nurs Midwifery Res, 1(2): 1-8.
Copyrights: ©2022 Makam CE, Adam A & Fusheini A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Abstract
Background: The dangers of self-medication, especially during pregnancy for both the woman and the fetus, have been extensively researched and documented.
Objective: The objectives of this study were to examine the prevalence of self-medication and associated factors among pregnant women in the Hohoe Municipality of the Volta Region.
Methodology: A descriptive cross-sectional design was employed to collect quantitative data from 371 pregnant women attending antenatal clinics in Hohoe Municipality. Descriptive statistics were used to analyze and present categorical data while bivariate correlation analysis was performed to determine variables associated with self-medication among pregnant women.
Results: The prevalence of self-medication was 62% among the participants. Herbal products (60%) and pain killers (51%) were the most used drugs for self-medication. Healthcare cost (r (269) = -.327, p=001), educational attainment (r(269)= .121, p= .020), and distance to the Municipal Hospital (r(269)= .121, p= .020) were factors that significantly correlated with self-medication. About 90% of the participants were aware and knowledgeable about the dangers of self-medication while pregnant.
Conclusion: High prevalence of self-medication among pregnant women with mostly herbal products was found. There is a need for culturally appropriate maternal health literacy programs to educate pregnant women about the dangers of self-medication while pregnant.
Keywords: Self-medication, Drugs, Pregnancy, Women, Ghana, Herbal, Medicine
INTRODUCTION
The practice of using medicine or medicinal products without medical consultations for various health or disease conditions has existed throughout history and continues to be followed globally, especially in deprived and rural communities. Different terminologies have been used to refer to the use of medicinal products for treatment and healing of various health conditions without prescription by a licensed physician across the world including drug or substance abuse. Technically, this is defined as the use of drugs to treat self-diagnosed disorders and symptoms or the intermittent or continued use of a prescribed drug for chronic or recurrent diseases or symptoms [1] or the use of manufactured or homemade drugs without a medical prescription to treat symptoms or self-diagnosed health conditions [2]. Many people in poor or developing countries and communities with limited healthcare resources and weak health delivery systems may rely on self-medication to take care of their health conditions. Self-medication is, therefore, one of the major healthcare decision initiation points when matters regarding safeguarding the health or treating an illness arise for many people around the world [3,4]. The global prevalence of self-medication ranges from 32% to over 90% [5]. Studies conducted in the United Kingdom and the United States have reported that an average of 50–75% of healthcare takes place within the realm of self-medication [6]. Additional studies have reported different prevalence rates in other countries [2,7,8]. Various reasons abound for self-medication in different parts of the world for different kinds of health conditions or perceived health conditions. Self- medication has been used for mood and anxiety disorders [9], sleep problems [10], and migraines [11]. In a cross-sectional study of self-medication among tertiary students in north-eastern Nigeria, 28% of participants reported themselves as having self-medicated to treat malaria as well as conditions such as ulcers, headaches, typhoid, pains (stomach/backache/menstrual pain), hypertension, diabetes, asthma, piles, and sexually transmitted diseases [12]. Other conditions such as fever, headache, dysmenorrhea, cough/cold, joint pain, constipation, diabetes, and allergies have been reported as health conditions that people self-medicate to treat [2,8,13]. In Ghana, a cross-sectional descriptive survey conducted at the Obstetrics and Gynecology department of the Komfo Anokye Teaching Hospital revealed that approximately 37% of the admissions for pelvic inflammatory disease (PID) and ectopic pregnancies reported self-medicating [14]. Other factors aside from direct health conditions have been reported as reasons for self-medication. These include ready access to drugs, socioeconomic factors, public health and environmental factors, demographic and epidemiological factors, lifestyle, increased potential to manage certain illnesses through self-care, and greater availability of medicinal products [15]. Other factors influencing self-medication practices have been reported, including disparities in healthcare systems such as reimbursement policies, access to healthcare, and drug dispensing policies, as well as age, sex, income, self-care orientation, education level in general and medical knowledge in particular, and exposure to advertisements [16]. It is important to note the various kinds of substances and medications that have been used for self-medication in various parts of the world. These include prescription drugs, over-the-counter (OTC) drugs, alcohol, herbal products, concoctions, and narcotics, among others. For example, alcohol and narcotic drugs have been used by many individuals with anxiety and mood disorders as a means of coping with their mental health conditions [17]. In a systematic review to identify and quantify the prevalence of self-medication with antibiotics in the WHO-designated South-East Asia Region, researchers reported antibiotics used in self-medication at a rate of 7.3% to 85.59%, with an overall prevalence of 42.64% in different countries across the region [18]. Other orthodox medications commonly used in self-medication have been reported, such as analgesics, vitamins, painkillers, and hematinics, including piroxicam, dipyrone, chloramphenicol, and many more [6,19]. In Ghana, self-medication is practiced by the majority of patients [20] and is highly prevalent in rural communities. This involves prescription drugs and herbal medicines and is sometimes a combination of both prescription medication and herbal concoctions [21,22]. Pregnant women of all ages and gestation constitute a vulnerable subpopulation and face specific health risks, and so engaging in self-medication has the potential to put them on the path toward jeopardizing their health and the health of their fetuses. For example, fetal alcohol syndrome, which encompasses the effects of fetal exposure to alcohol during pregnancy; has been extensively researched and reported on. However, just as it has in the general population, self-medication has also been reported among pregnant women in many parts of the world. Research has shown that self-medication is as common among pregnant women as it is among the general population, and varied reasons have been given by pregnant women for engaging in self-medication [13]. In a study in two municipalities in the Central Region, Ghana, researchers reported 69% of 136 pregnant women self-medicated [23]. Also, in a study of 372 pregnant women in the Mwanza Health Centre in Tanzania, researchers noted that 46% reported themselves as having self-medicated, with unemployed and homemaking pregnant women being more prone than employed women to engage in self-medication [24]. Two studies in Jos [13] and Jos-North [25] in Nigeria respectively reported a self-medication prevalence of 85% and 63% among pregnant women attending antenatal clinics. Self-medication among pregnant women is a potentially dangerous practice for both pregnant women and their unborn babies. Though extensively studied, there has not been much focus on self-medication and its associated factors and health outcomes among pregnant women in Ghana and in the Hohoe Municipality in particular. The main objective of this descriptive cross-sectional study was, therefore, to assess the prevalence of self-medication and its associated factors among pregnant women attending various antenatal clinics in the Hohoe Municipality of the Volta Region of Ghana. In addition, we examined knowledge of dangers of self-medication while pregnant among the pregnant women.
METHODS
A descriptive cross-sectional study was conducted using a structured questionnaire to collect data on self-medication and knowledge of risks associated with self-medication during pregnancy among pregnant women in the Hohoe municipality of Volta Region of Ghana.
Setting and target population
The study was conducted in the Hohoe Municipality of the Volta region which consists of ninety - two (92) communities with a projected population of 188,962(52.1% female and 47.9% male) in 2016 from the 2010 Population and Housing Census (PHC) [26]. From the data, women of their reproductive ages (15-49) constituted 25.4% (n=47,996) of the population of the Municipality. The Municipality has a total of 21 health facilities but for this study, six health facilities were conveniently selected including Hohoe Municipal Hospital, Gbi-Wegbe Health Centre, Lolobi-Kumasi Health Centre, Likpe Bakua Health Centre, Alavanyo Wudidi Health Centre, and Hohoe Adabraka Health Centre. The target population for this study included all pregnant women who were living in the Hohoe Municipality at the time of the study. The inclusion criteria were that a woman confirmed pregnant regardless of the gestation of the pregnancy, living in the Hohoe municipality, attending antenatal clinic in the Hohoe municipality, and had to willingly and voluntarily agreed to participate in the study.
Sample size determination and sampling of participants
The exact population of pregnant women in the Hohoe municipality was not known since not all pregnant women register for or attend antennal services. Therefore, to determine the sample size for this study, a sample determination formula by Kothari [27] which is widely used was adopted. The parameters were set at a 95% confidence interval and a response distribution of 50%. From the calculations, the recommended sample size was 338 but we added 33 (10%) non-response rate to the recommended 338 to ensure we had the required sample size. This brought the sample size to 371 participants.
Sampling method
A combination of convenience and systematic sampling was used to recruit health facilities and pregnant women into the study. Convenience sampling was used to select six health facilities after examining their enrolment and attendance data at their antenatal clinics and the fact that they provided the standard antenatal care services. The six health facilities are also conveniently spread out in the municipality for which results from the study may be generalized. The selected health facilities included Hohoe Municipal Hospital, Gbi-Wegbe Health Centre, Lolobi-Kumasi Health Centre, Likpe Bakua Health Centre, Alavanyo Wudidi Health Centre, and Hohoe Adabraka Health Centre. At the various health facilities, participants were selected using systematic sampling after administrators introduced the researchers and the researchers explaining the purpose and nature of the study to the participants. The sampling frame of each health facility was examined using antenatal clinic enrolment data and proportionate numbers were assigned to each facility. A sampling interval was then created at the health facilities for the days that data collection was done and used to select participants voluntarily into the study until the required sample size was attained. The number of participants recruited from the health facilities differed with a larger majority recruited at Hohoe Municipal hospital. The rest of the five health facilities had relatively even distribution of participants.
Data collection procedure and analysis
The data for this study were collected using semi-structured questionnaires designed for the study. The questionnaire was written in the English language at a basic education comprehension level. The majority of the participants was literate and could read and understand the questions and so self-administered the questionnaires in the presence of data collectors. However, the questionnaire was verbally translated for respondents who had no formal education and those who had difficulty reading and understanding the questions into Ewe, the local language spoken by over 90% of the population of Hohoe Municipality. The data collected covered socio-demographic variables, the practice of self-medication and associated factors, and data on types of drugs and substances used for self-medication. Data on knowledge of dangers associated with self-medication in pregnancy as well as types of complications that could result from self-medication were also collected. Before collecting data, the questionnaire was pretested with selected pregnant women at the various health facilities and minor corrections were made. Also, terminology that appeared too technical was changed into lay terms and explained. The women who participated in the pretesting of the questionnaire were noted and were not included in the actual data collection exercise. For confidentiality and anonymity, the names of the respondents were not included in the questionnaire. The data were entered into Epi info 7.1 and exported into SPSS version 22. The data were cleaned in SPSS as well to detect missing values and make the necessary corrections. Descriptive statistics were used to analyze and present data on the socio-demographic variables and other categorical variables in frequencies and percentages. Bivariate correlation analysis with Pearson chi-square was performed to determine the variables that had a statistically significant relationship with self-medication among the pregnant women in this study.
Ethical review and approval were obtained from Ghana Health Service Ethical Review Committee (GHSERC). The ethics approval was granted in May 2017, with reference number GHS-ERC: 28/05/17. Additionally, the Hohoe Municipal Health Directorate, and the Hohoe Municipal Hospital granted permission before the data were collected between December 1st 2017 and February 28th 2018. During the data collection, each participant was provided with a study information sheet that introduced the researchers and explained in detail the purpose, procedures, benefits, and risk for participation. The information sheet also explained the confidentiality of information, data management, and storage besides clearly informing the participants that their participation was completely voluntary and that no penalty whatsoever existed for their refusal to participate. Each participant was also given an informed consent form and it was only those who voluntarily agreed to participate in the study by either signing or thumb printing the informed consent who were recruited into the study. The questionnaires were coded with identification numbers and so names or personal identifiers were not put on the questionnaire to ensure the anonymity of the participants. However, girls (within the ages of 12 to 17 years) who were pregnant, participated after they signed an assent form and their parent/guardian also signed an informed consent form on their behalf.
RESULTS
Socio-demographic characteristics of participants
A total of 371 pregnant women participated in this study. The mean age of the participants was 27 (SD=6.40) years. The majority, 203 (54%) of the participants fell into the age group 20-29 years. There were 44 (12%) teenagers aged 15-19 years, and 51 (14%) women aged 35 years or more. The majority, 265 (71%) reported being married. About 95% had least primary education, and the majority of the respondents, 325 (88%) were Christians. Only 58(16%) of the participants reported being unemployed. The majority (60%) of the participants were recruited from Hohoe Municipal hospital while the other 40% was distributed fairly even among five health centers across the municipality.
Prevalence of self-medication among the pregnant women
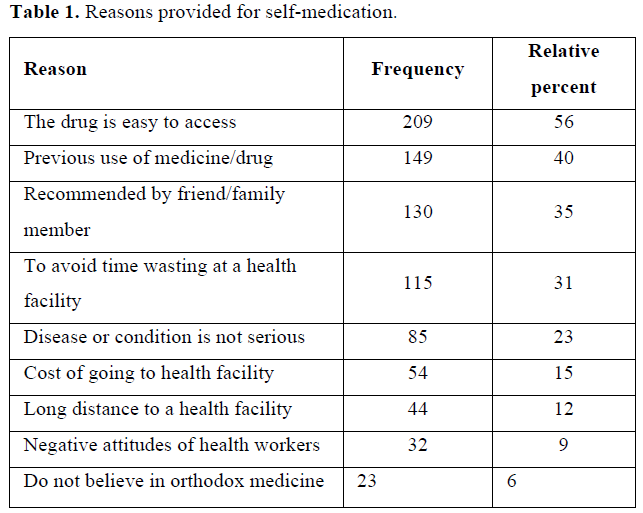
Out of 371 pregnant women, the majority [228 (62%)] reported that they self-medicated while pregnant. The reasons advanced for self-medication among pregnant women are presented in Table 1. The availability/ease of access to various drugs was the most common reason provided influencing the practice of self-medication. Previous experience with self-medicated drugs, the drugs being recommended by friends and relatives, time-wasting at a health facility, and disease perceived as a minor illness were also common reasons given for self-medication.
To determine the variables that showed statistically significant associations with self-medication among the pregnant women, bivariate correlations with Pearson coefficient was performed. Pearson correlation results showed that three variables including the perception of healthcare cost (r (269) = -.327, p=001), distance of participants to the Municipal Hospital (r(269)= .121, p= .020., and educational attainment(r(269)= .121, p= .020) of the participants had statistically significant association with self-medication. We then developed a model using multiple regression analysis to determine variables that significantly predicted self-medication among the study sample with self-medication as dependent variables and the socio-demographic variables as predictor variables. The results show that only education (P= 0.01) and distance from municipal hospital (P=0.02) significantly predicted self-medication among the participants. The results are in Table 2.
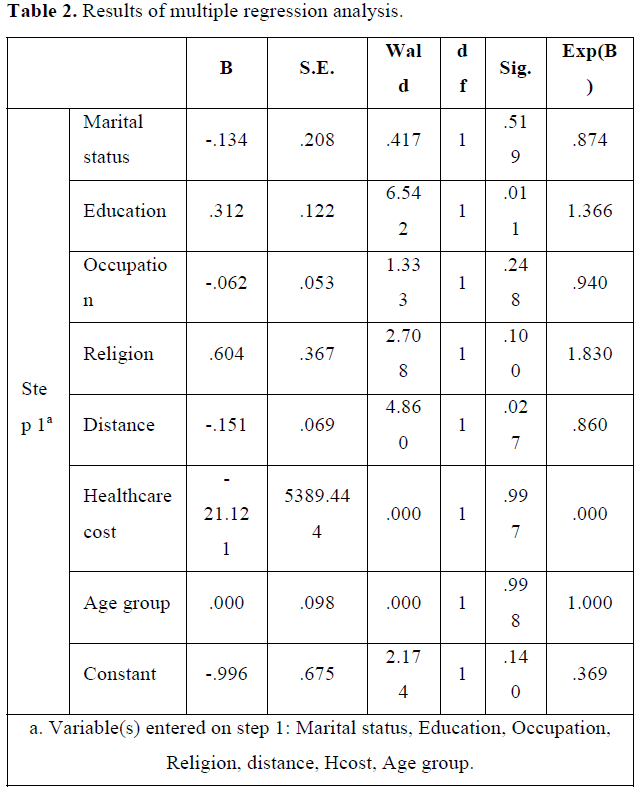
To know the exact relationship the education and distance from Hohoe municipal hospital had with self-medication a two-by-two contingency analysis was performed for each of the variables against self-medication. The results also showed that the farther the distance of the participant from Hohoe Municipal hospital or township, the higher the likelihood to engage in self-medication. Finally, the results showed that those with lower educational attainment were highly likely to engage in self-medication than those with higher education. For instance, 72%, 67%, 59%, and 34% of those with primary, JHS, SHS, and tertiary education engaged in self-medication respectively.
Drugs used for self-medication among pregnant women
The participants who reported self-medicating above used various types of drugs, medication, and/or substances during their pregnancies. Herbal products or medicine were the most used by 136 (60%) of the 228 who self-medicated. Analgesics of various brands were the next with 116 (51%) of the women using them. Cold medicines and anti-diarrheal drugs were used by 19 (8%) and 15 (7%), respectively. Antibiotics and anti-malaria drugs were used by 9 (4%) and 11 (5%) women respectively.
Diseases and conditions treated through self-medication among pregnant women
Anemia was the most-cited condition among the pregnant women, involving 104 (46%) out of the 228 women who self-medicated. Others were headaches [98 (43%)], pain-related conditions, including waist, body, and abdominal pains [91 (40%)], malaria (23%), nausea (14%), cough/fever (10%), diarrhea (6%) and dizziness (3%).
Awareness/knowledge of effects of self-medication in pregnancy
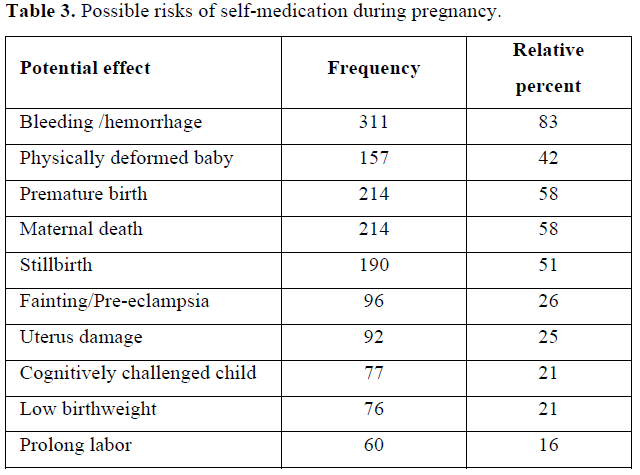
The majority [334 (90%)] of the pregnant women reported being at least aware of possible negative outcomes of engaging in self-medication while pregnant. Participants were further asked to name some negative outcomes that they knew could result from self-medication. The responses are presented in Table 3.
DISCUSSION
The findings from this study show that the study group was a largely youthful, literate, and occupationally stable population.
Prevalence of self-medication among pregnant women
A high prevalence of self-medication (62%) was recorded among pregnant women. This prevalence is higher than the 36% reported in the East Mamprusi District of the Northern Region of Ghana [27] but lower than 69% reported in the central region of Ghana [24] and 76% reported among women in Iran [28]. This finding is also consistent with the generally high prevalence of self-medication in the larger Ghanaian population [21,29] and elsewhere [2,5-714,30]. Similar rates of high prevalence of self-medication have been reported in other African countries [19,31,32]. The differences in the rates of self-medication above may be due to differences in socio-cultural and economic factors. However, the finding of a high prevalence of self-medication seems to be a reflection of the prevalence of self-medication in the general populations of Ghana and other sub-Saharan African countries.
Reasons influencing self-medication practices among pregnant women
Another objective was to examine the factors that influenced self-medication among pregnant women in this study. The major reasons provided by the participants for engaging in self-medication included easy access to various medication/substances (56%), previous use of the medication (40%), family/friend recommendation (35%), illness considered mild (23%) and healthcare cost (15%). These findings are similar to findings from other researchers where easy access to various drugs and the cost of healthcare were major factors in self-medication in Ethiopia, Nigeria, and in the United States [2,19,33]. For instance, in a similar study in Ethiopia, researchers found that a plurality of the respondents (45.9%) indicated easy access to drugs as their reason for practicing self-medication [2]. Other findings revealed that unrestricted or easy access to drugs was the most common reason for respondents engaging in self-medication during pregnancy [19,27,34]. The influence of friends and family members on self-medication among pregnant women reported in this study is also consistent with other findings from other studies [19,28].
However, in a binary logistic regression model analysis, only educational attainment of the participant (r (6.542) = .1, p= 0.01), and distance or location from the participant to the Municipal hospital (r (4.860) = .1, p= 0.027) were factors that significantly correlated with self-medication. Pregnant women who an educational level lower than SHS, and those who lived outside or far from the municipal capital, Hohoe, were more likely to self-medicate than those with SHS education or higher and those who lived in close proximity to the Municipal hospital. The finding of location/residence and educational level as predictors of self-medication is consistent with findings from similar studies [23,24,35] elsewhere.
Drugs that are often self-medicated during pregnancy
With regards to the medicines or substances used in self-medication, two major drugs/substances were reported, including herbal substances and analgesics (painkillers). From the results, 136 (60%) and 116 (51%) of the 228 who self-medicated used herbal products and painkillers respectively to self-medicate. This makes herbal products the most commonly used to self-medicate by pregnant women in the Hohoe Municipality. The finding is inconsistent with a recent and similar study in the Central region in which researchers reported antibiotics (32%) as the most common [23]. It is, however, consistent to the extent of the finding of painkillers as the second most common drug category used for self-medication among pregnant in both studies. The difference in these settings may be due to different socio-cultural as well as economic factors. For instance, Hohoe Municipality is a largely rural society, except Hohoe township, where many people live traditional lives and rely on herbal products for their health maintenance, and it is a major market for the production and selling of herbal products. Other studies have reported the use of herbal products and/or painkillers for self-medication in the literature corroborating our findings [16,27,34-37]. However, it is important to note that the use of antibiotics anti-malaria drugs and hematinics (blood topic) for self-medication by respondents was relatively low in this study involving less than 10% of respondents. This is inconsistent with many other findings in Ghana and outside Ghana [2,14,23,28,34]. For instance, in a systematic review, researchers found antibiotic use for self-medication to be between 7.3% and 86% in the WHO Southeast Asia region [18]. A closer examination of the findings with regards to the drugs and substances used for self-medication indicates that a mixture of different medications or substances may have been used in self-medication, simultaneously putting the health of the pregnant women and their unborn babies at greater risks of negative outcomes. For instance, 60% and 51% of those who engaged in self-medication used herbal products and analgesics, respectively. Some of those who self-medicated with herbs may have also self-medicated with analgesics, thereby increasing the risks of pregnancy complications and negative birth outcomes.
Diseases/conditions for which drugs were self-medicated
The variety of ailments for which self-medication was applied included anemia, headaches, pain-related, and malaria. The finding appears to coincide with high prevalence of anemia among pregnant women in the Hohoe Municipality and Volta region in general. In a study to determine the prevalence of malaria and anemia among 1200 pregnant women in the Hohoe Municipality, researchers found 60.3% prevalence of anemia [38]. Self-medication to treat headaches is consistent with findings from other studies where headache/fever was the most common self-medicated illness, as reported in a similar study in Nigeria [14,27]. Pain-related conditions including body, abdominal, and waist pains were in line with the findings of a similar study in Nigeria [27,31,34]. What these findings means for clinical practice is that there is the need for clinicians at the ANC clinics to pay more attention to these conditions and engage pregnant women on how best to manage their symptoms using safe prescribed medication and nutrition.
Awareness of the dangers of self-medication during pregnancy
An important element in this study that we found scanty literature on was whether or not the pregnant women in this study were aware or had knowledge about the dangers posed by self-medication while pregnant. The overwhelming majority 334 (90%) reported that they were aware. We found that knowledge of the dangers of self-medication with pregnancy was significantly correlated with the educational level attained. The major complications listed by the women as potential dangers associated with self-medication in pregnancy included bleeding (hemorrhage), premature birth, maternal death, stillbirth and physical deformity of babies. Other serious complications were listed and these clearly show that the women in this study were at least aware of serious maternal health issues. The finding is inconsistent with the only finding we found in a study in the Greater Accra Region in Ghana where the researchers reported that 82% of 361 participants did not know the dangers of self-medication. The difference in the awareness/knowledge of the dangers of self-medication in the two studies could be the result of differences in the socio-demographic difference in the two studies. For example, while 95% of the women in our study had attained at least primary education, only 44% of the sample in another study had primary education as the highest education attained. Other researchers have reported knowledge of the consequences of self-medication while pregnant [13,25]. Health educators and dieticians at these clinics may need to include educational programs and easier to understand information about self-medication and its attendant dangers for pregnant women and the unborn babies.
LIMITATIONS
The major limitation we encountered during this study was time constraints on the part of the pregnant women who participated in the study. The women visited the health facilities for antenatal care services and their minds were focused on receiving services first. We, therefore, had to wait for them to be attended to by the nurses before administering the questionnaire. The questionnaire had to be administered quickly as many of the pregnant indicated they had other commitments to attend to. Also, even though the questionnaire was pretested and improved, a small proportion of the pregnant women had challenges understanding the questions as it was written in English language. Therefore, some questions had to be explained to the few women who had difficulty understanding in Ewe, the local dialect spoken by over 90% of the residents in Hohoe Municipality. Despite these two challenges, every effort was made with care to accommodate the time limitation of the mothers and to accurately explain the questions in plain language to mitigate any negative effects on the quality of data collected.
CONCLUSION
Self-medication during pregnancy is a serious public health issue in the study population. Herbal products and analgesics were the most commonly employed agents and the commonest illnesses addressed were anemia, and headaches. Low educational attainment and distance to health facilities were significantly associated with self-medication. The findings show a high prevalence of self-medication among pregnant women in the Hohoe Municipality and surrounding areas.
REFERENCES
No Files Found
Share Your Publication :